Biotechnology and the next pandemic part 1: Historical biothreats
Faouzi Braza & Ashley Noriega | July 2024
This article is the first of a three-part series discussing the potential role of biotechnology misuse in the emergence of the next pandemic.
Here we will outline the state of the art knowledge of pandemic and biothreats and introduce the risks posed by emerging technologies. The second part of this series will discuss and outline how the convergence of synthetic biology and artificial intelligence may critically challenge our current biosecurity policy landscape. Finally, the last article will focus on the state of preparedness of Europe against this evolving threat landscape.
Introduction
As the world emerged from the onslaught of the COVID-19 pandemic the question for policymakers has naturally turned to the future likelihood of a similar event. A study from 2022 examined a global dataset of historical epidemics from 1600 to 1945. 385 epidemics were compiled and examined to estimate the probability of extreme epidemics occurring in a given year. The study found that there is a 17% chance of facing a COVID-19 like event.
This calculation gained significant attention, somewhat overshadowing an even more eye-catching finding: this 17% chance could jump to 44% taking into account the continued impact of human activities on our planet. Phenomena including deforestation, urbanisation, and climate change are massively altering and reshaping ecosystems worldwide. These changes alter the landscape of infectious diseases and create new opportunities for diseases to spread more rapidly. This phenomenon sets the stage for more frequent and severe epidemic outbreaks with massive societal and economic impacts.
One of the unexpected long-lasting impacts of the COVID-19 pandemic has been the significant increase of public awareness of biological sciences and of the societal and health impacts of pandemics. For several years, the media and political spheres were filled with debate on the origin of the virus and of the capability of biotechnology research to engineer pathogens, quickly prompting discussions about the ethical implications and regulatory frameworks necessary to prevent future accident and misuse. Now, concerns about natural outbreaks are intertwined with fears of intentional release or accidental man-made pathogens that may cause the next global pandemics. But how real is this threat?
Pathogens as an agent of war
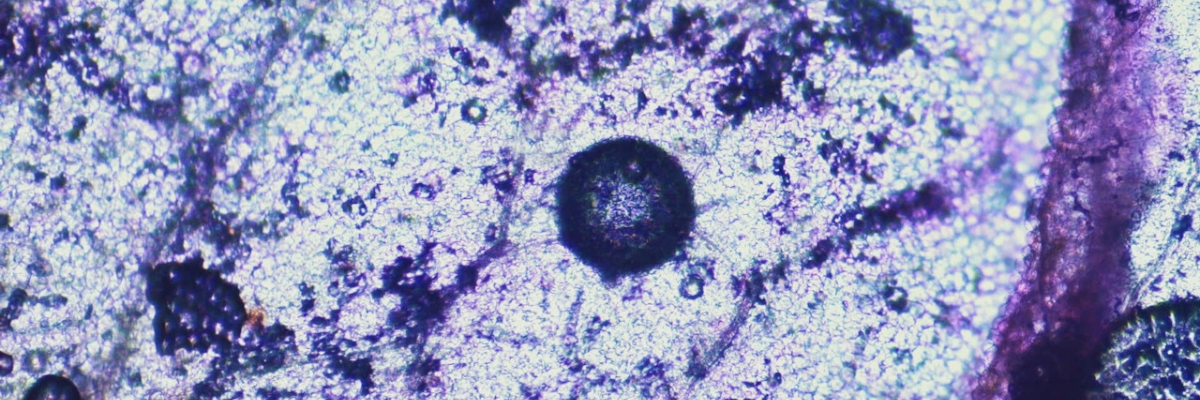
The use of microorganisms as an agent of war is extremely old, dating back to the Mongols’ use of plague-stricken corpses to infect the population defending the besieged city of Caffa in 1346. Since then, a number of microorganisms have been configured for use as biological weapons.
The Biological Weapons Convention was agreed in 1972 to “prohibit the development, production, acquisition, transfer, stockpiling and use of biological and toxin weapons”. It raised hopes that pathogens would no longer be used as weapons of war. However, it was later discovered that the Soviet Union had continued its bioweapons development program despite signing the convention. The Soviet Union’s efforts were vast and astonishing in scale: they manufactured and stockpiled large quantities of anthrax bacilli and smallpox virus, some intended to be used in ballistic missiles. They also engineered multidrug-resistant bacteria, and conducted research on haemorrhagic fever viruses that are among the deadliest pathogens known to humanity. It was only in 1992 that Russian President Boris Yeltsin acknowledged the existence of this bioweapon research military program1.
After the Soviet Union collapsed, many of these programs were discontinued, and the research facilities were either abandoned or repurposed for civilian activities. However Western security experts now express concern that some stockpiles of biological weapons may not have been destroyed and could have ended up in unauthorised hands. At the global level, U.S. intelligence reports that several nations have either developed or are still pursuing biological weapons. Both China and the United States have also recently acknowledged that threats enabled by the last decade of biotechnology advancements need to be addressed in order to preserve national security.
Military defence is primarily a national competency within the European Union, meaning that individual member states retain sovereignty over their defence policies. However, the European Commission plays an increasingly important role in fostering defence cooperation notably through the European Defence Agency (EDA). The EDA drives defence cooperation against the chemical, biological, radiological, and nuclear threat mainly through international cooperation with partners like NATO.
Pathogens as a weapon of terrorism
Biological warfare has long been thought of as the domain of nation states, but a number of incidents have demonstrated how individuals and non-governmental groups have also gained access to dangerous pathogens:
One notable case involves a religious sect in the United States, which attempted to poison an entire community by contaminating salad bars with Salmonella in 1984, with the aim of disrupting a local election. 751 people were infected and 41 were hospitalised. The sect, which operated a hospital, was able to acquire the bacterial strain from a commercial supplier.
Another famous example comes from the 1995 Sarin gas attack in the Tokyo subway, committed by the Aum Shinrikyo’s religious cult. The release of this toxic compound resulted in the deaths of 12 passengers and injuries to over 6,000 others. Prior to this attack, the group had made several attempts to produce and spread anthrax and botulinum toxin. They had failed despite having set up a fairly advanced biomanufacturing process.
So far, bioterrorist attacks have been primarily constrained by two limiting factors. First, lack of available research talent. Non-expert actors do not have the necessary experience and knowledge accrued through years of biological research to develop dangerous microorganisms. Second, the relevant infrastructure. The manipulation and production of dangerous pathogens requires specialised containment facilities to protect individuals from the effects of agents being used.
But those two limiting factors are becoming less and less relevant. Paul Riley, an expert on preparedness specialising in biosecurity and biosafety at the European Center of Disease Control (ECDC), recently underlined how “COVID-19 opened people’s eyes on how impactful an outbreak of infectious disease could be” and suggested that terrorists might investigate ways to leverage this impact. He also highlighted how “the technologies are also improving today” giving the example of garage scientists who have seen their capabilities increased thanks to major technological advances in biotechnology. This is particularly concerning as biological weapons can be produced at a fraction of the cost of conventional arms—up to 2,000 times cheaper—while remaining equally effective.
Major terrorist attacks in the last decades prompted the EU to become an increasingly important actor in counter-terrorism. Member states have adopted several ambitious programs and policies, including the “Anti-terrorism Roadmap”, the “EU Plan of Action on Combating Terrorism” and the “EU Counter-terrorism strategy”. However, measures designed to counter risks posed specifically by emerging biotechnologies are still undefined.
Pathogens as an unintentional threat
While intentional manipulation by nefarious actors remains an area of concern to policymakers, it is worth remembering that human and technical errors have been the main cause of the release of high-risk pathogens throughout history.
In 1955 an error in the production process of polio vaccine was responsible for the “Cutter Polio Vaccine incident” that led to the death of 10 children and 164 hundred cases of paralytic polio. In 1979, it was a defect of the lab’s ventilation system that caused the expulsion of a weaponized version of Anthrax in the surroundings of a local Russian city leading to the death of hundreds of people. In 2019, infected aerosolized particles from the Lanzhou pharmaceutical company in China were identified as the source of the first cluster of human cases of a Brucellosis outbreak. It was reported that an expired disinfectant for cleaning was the root cause of this accident. Luckily, no deaths were reported among the 10,528 infected people.
A comprehensive analysis showed that 72% of high-risk pathogens release events reported from 1975 to 2016 were accidental. Historical data tells us that pathogens are occasionally released from controlled environments; the vast majority of the time this is accidental – and, critically, through a combination of factors including built-in biosafety measures these events have not escalated into major pandemics.
To control risk from accidental lab leaks, the EU proactively designed, implemented, and refined a comprehensive set of biosafety regulations. Each EU member state is obliged to implement these regulations in their national legislation’s corpus. Some regulations require laboratories and other entities handling disease agents to protect professional workers from the exposure of biological agents (Directive 2000/54/EC) and to apply adequate biosafety and biosecurity measures (Regulation (EU) 2016/429). However, despite ongoing international negotiations for a global pandemic accord, establishing rules and an enforcement system for a harmonised global biosafety ecosystem remains elusive.
When reflecting on the overarching threat posed by dangerous pathogen leaks from laboratories, it is important to consider that the threat relates to the number of facilities handling these pathogens. Analysis of the probability of such incidences estimates that for every laboratory handling dangerous materials, there is a 0.2% likelihood of the escape of a high-risk pathogen per year.
If we imagine that there are 10 laboratories working with high-risk pathogens over the course of 10 years, this likelihood is increased to 18%. In line with previous modelling, the ability of COVID-19 to spread and the estimated number of laboratories handling highly dangerous pathogens worldwide, the likelihood of a laboratory leak event turning into a pandemic in the next 100 years could be as high as 36%.
In 2010, the US National Research Council evaluated the risk of a laboratory leak happening at the National Bio- and Agro-Defense Facility (NBAF) in Manhattan (Kansas). They notably qualified previous estimations to be “overly optimistic”, with “unsupported estimates of human error rates”. They estimated the likelihood of a leak happening at the NBAF to be around 70% for the 50-year life of the facility which would correspond to a likelihood of 2.3% per year. This is significantly higher than other laboratory leak scenarios at 0.2%. If we translate this assessment into a global context, this increases the likelihood of one pathogen escaping from 10 labs in 10 years to 91%.
Conclusion
Recent projections presented at the 2024 Copenhagen Democracy Summit in Copenhagen drew an alarming picture: a 27.5% chance of a COVID-19-like pandemic occurring in the next decade. The scenarios under which such an event could materialise range from intentional or accidental pathogen release, to naturally occurring animal-human transmission. Here, we have considered the weaponisation of microorganisms, the probability of these escaping a laboratory environment and how these events might lead to a global pandemic. These can all be thought of as drivers of risk.
Understanding risk and accepting uncertainty are perennial challenges for decision-makers. Understanding the drivers of risk can help policymakers to create future proofed strategies and systems.
A further driver of these risks is the speed and spread of developments in the field of biotechnology, namely anyone with an internet connection now has access to open-source databases that contain extensively annotated genomic sequences across all virus families, is able to order synthetic DNA from companies internationally, and shop online for molecular biology tools. We explore the questions of accessibility and technological capabilities in Part 2 of ICFG’s series on biothreats.
It is logical, then, that good governance of developments in biotechnology is a vital part of safeguarding against the risk of bioweapons. As these technologies improve and become more accessible outside of regulated research laboratories, more groups could potentially use them to cause widespread damage.
Despite these trends and the massive shock of the COVID-19 pandemic, biosecurity is a notable gap in the EU’s portfolio. This is in contrast to the United States, which has outlined a comprehensive approach in its recent US Biodefense Posture Review to address the evolving threat landscape posed by the convergent advancements observed in biotechnology and artificial intelligence. Recognizing these gaps, we, at ICFG, have called for the European Commission to adopt a comprehensive EU Biosecurity Strategy that clearly outlines mechanisms to bridge existent and missing EU competencies in research, health, and defence ensuring the EU is better equipped to counter the increasing threat of bioweapons.
1 Countries such as the US, UK, South Africa, Israel, and Iraq have all pursued the development of biological weapons at various points in history. However, obtaining up-to-date information remains a significant challenge, as the covert nature of these programs makes detection and identification notoriously difficult.
